A 52 yr old female ,homemaker by occupation
http://keelasreevalli.blogspot.com/2021/09/a-52-yr-old-female-homemaker-by.html
CASE :
A 52 year old female,house wife resident of narketpally came to the causality in a drowsy state
She was apparently asymptomatic 1 week back,when she sustained an injury to the left LL(shin according to attenders but wound not visible outside -outside x-rays normal ),after which she developed pain and edema ,she was treated outside with pain killers ,had restricted movements and hence did not move much and lied on bed most of the time ,walked with support and gradually the swelling got decreased to some extent . 5 days later she again visited RMP as her appetite was decreased and also associated with generalised weaknesses and left lower limb pain and also hip( localisation not possible )for which pt was given IV fluids and pain killers.
This morning after eating ,she had sudden onset of around 10-15 vomiting episodes with nausea then she suddenly became drowsy ,while she was being shifted here,there is irrelevant talk and pt was incoherent.
On presentation, pt was unconscious with
E1V1M4 to E1V1M1
Past history :
No H/o diabetes, hypertension,asthma epilepsy,TB
No similar complaints in the past
No history of any surgeries or blood transfusions
Personal history :
Diet - Veg
Appetite - decreased
Sleep - adequate
Bowel and bladder movements : Regular
No known allergies
No history of alcohol consumption or smoking
On examination:
Pt is stupourous ,withdrawal from pain
Febrile to touch:100°F
PR: 86bpm
BP: 130/70 mmHg
RR: 24
CVS: S1, S2 heard
RS: BAE present ,end inspiratory wheeze in all areas ,
Spo2: 96%on room air
P/A: obese ,non tender ,bowel sounds sluggish
CNS:
Pupils - right side -NS RL
Left side - post cataract surgery r/n to light
Gag present
Tone : normal b/l
Reflexes
Lt. Rt
B. 2+. 2+
T. 2+. 2+
S. 2+. 2+
K 2 +. 2+
A. 2+. 2+
P. Upgoing. Upgoing
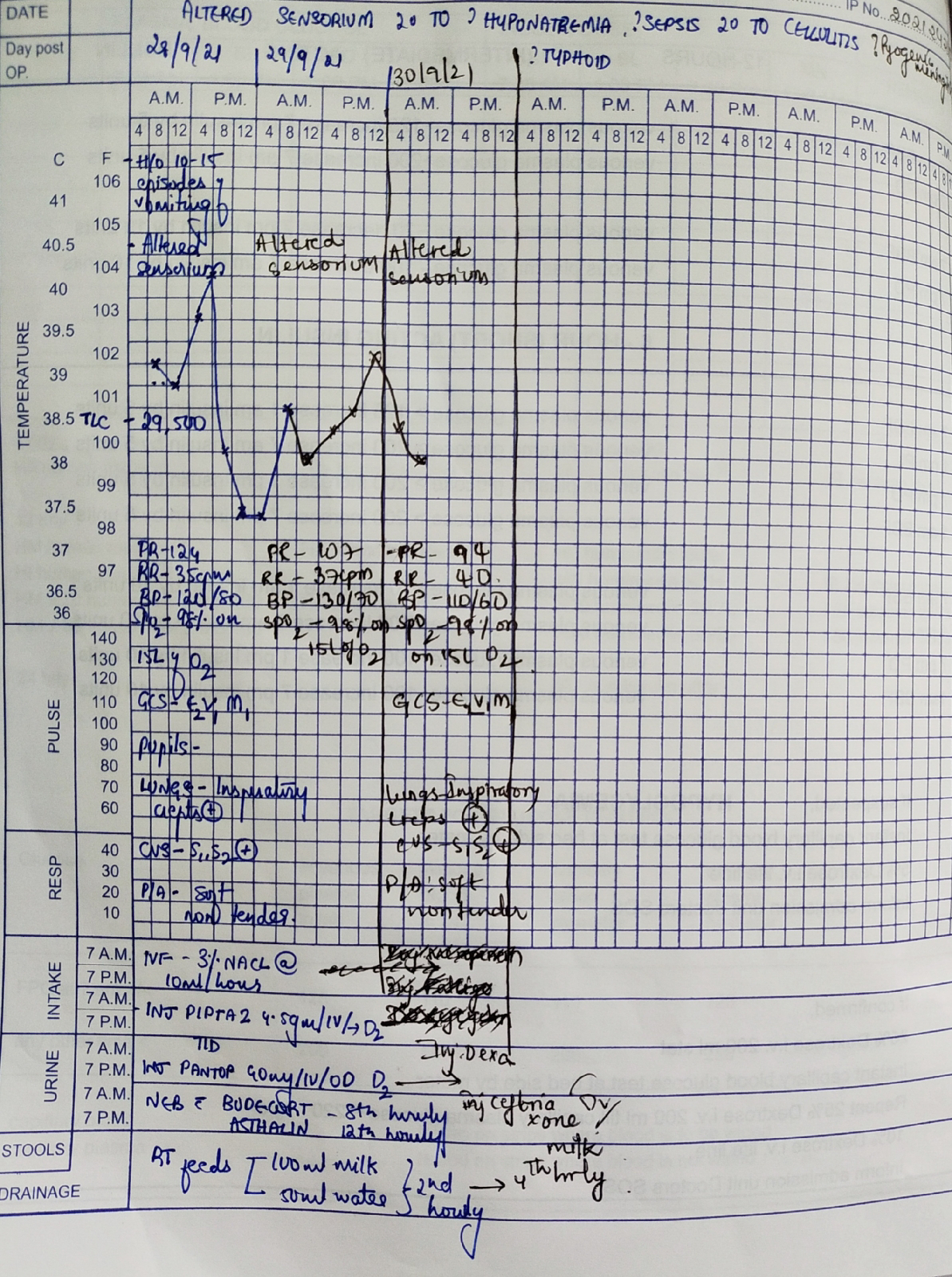
Provisional diagnosis:
Altered sensorium under evaluation secondary to hyponatremia( euvolemia)?SIADH
Sepsis secondary to ?cellulitis ? Typhoid
with complete right bundle branch block
Investigations :
RFT :
Urea - 15
Creatinine - 0.6
Uric acid - 2
Calcium - 8.6
Phosphorus - 3.2
Na+ : 118
K+ : 3.8
Cl- : 76
LFT :
TB : 0.88
DB : 0.20
AST : 26
ALT : 13
ALP : 177
TP : 5.5
ALB : 3.1
A/G : 1.33
Serum osmolality :
Serum sodium @ 10pm
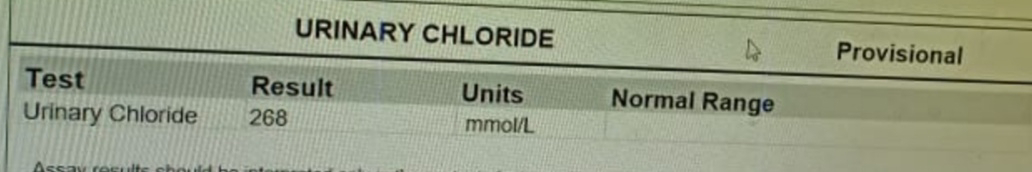
Urinary electrolytes :
ECG :
CHEST X RAY :
MRI BRAIN :
TREATMENT :
1) Propped up position
2) IVF 3% Nacl @10 ml/hr
3) Ryles catheterization
4)Foley's catheterization
5)Inj.Piptaz 4.5 gm /IV/BD
6) RT feeds : 100ml water 2nd HRLY
50 ml milk 4rth HRLY
Day 2 of admission :
Pt is stupourous ,withdrawal from pain
Febrile to touch:100°F
PR: 86bpm
BP: 130/70 mmHg
RR: 24
CVS: S1, S2 heard
RS: BAE present ,end inspiratory wheeze in all areas ,
Spo2: 96%on room air
P/A: obese ,non tender ,bowel sounds sluggish
CNS:
Pupils - right side -NS RL
Left side - post cataract surgery r/n to light
Gag present
Tone : normal b/l
Reflexes
Lt. Rt
B. 2+. 2+
T. 2+. 2+
S. 2+. 2+
K 2 +. 2+
A. 2+. 2+
P. Upgoing. Upgoing
Diagnosis:
Altered sensorium under evaluation secondary to hyponatremia( euvolemia)?SIADH
Sepsis secondary to ?cellulitis ? Typhoid
with complete right bundle branch block
Investigations :
RFT :
Urea - 13
Creatinine - 0.6
Uric acid - 2
Calcium - 8.5
Phosphorus - 3.5
Na+ : 128
K+ : 3.9
Cl- : 90
ABG :
Electrolytes @ 2pm :
Na+ : 123
K+ : 3.9
Cl- : 85
Electrolytes @10 pm :
Na+ : 123
K+ : 3.9
Cl- : 85
Pt developed bed sore on her right
buttock :
Treatment :
1) Propped up position
2) IVF 3% Nacl @10 ml/hr
3) Inj.PANTOP 40 mg PO/OD
4)Inj.Piptaz 4.5 gm /IV/TID
5) Nebulization with budecort @ 8th HRLY and
Asthalin @12th HRLY
6) RT feeds : 100ml water 2nd HRLY
50 ml milk 4rth HRLY
Day 3 of admission :
Still in altered sensorium
And attendant complaints of her having on and off fever episodes and no improvement in sensorium since admission
O -
However her GCS has gone up from E1M1V1 to E2V1M1
RR - 35 cpm
PR - 124bpm
BP- 120/70mmhg
Temp - 101 F
Spo2 - 98%on 15L RA
CNS -
E2M1V1
Pupils -
Bilaterally reacting to light
Left post cataract surgery
Hypotonia + in all 4 limbs
Reflexes-
Bilateral biceps +
Plantars - Mute
Corneal and conjunctival reflexes +
No meningeal signs
Lungs - Bilateral inspiratory crepts in all Lung fields
And expiration wheeze in all Lung fields
Cvs - S1,S2+
Per Abdomen - soft
Bowel sounds +
A -
Altered senorium secondary to ? Hyponatremia
Sepsis secondary to ? cellulitis
? Typhoid
With complete RBBB
P -
LP was done will be updating shortly
Continuing her on
Inj 3% NACL @ 10ml/hour
Inj Pantop 40mg IV OD
Inj Piptaz 4.5 gm/IV/TID
Neb with budecort 8th hourly and Asthalin 12 hourly
RT feeds - 100ml milk and 50ml free water 2nd hourly
Tab Dolo 650mg sos
Hemogram :
Hb - 11.6
TLC : 46500
Plt : 39900
RBC : 4.56
ABG @ 6am :
Chest xray :
ECG :
ABG @ 12pm :
After lp,csf was sent for analysis :
Volume : 1ml
Appearance : clear
Color : slightly reddish
TC - 436 (corrected WBC count )
Dc - 90% neutrophils ,10% lymphocytes
RBC - 14650
Others : nil
Awaiting cytology reports
Csf sugar : 25
Csf protein : 29
Csf chloride : 116
RBS : 85
Electrolytes @6pm :
Na - 122
K - 4.2
Cl - 80
Day 4 :
52 year old woman,
ICU bed 1
Still in altered sensorium
And attendant complaints of her having on and off fever episodes
no improvement in sensorium since admission
O -
GCS E2V1M1
Pt is on mechanical ventilation
Simv - vc mode
Tv - 400 ml
PEEP - 5 cm of h20
FiO2 - 30%
RR - 40 cpm
PR - 94bpm
BP- 110/60mmhg
Temp - 37.3 C
Spo2 - 98%on 15L RA
CNS -
E2M1V1
Pupils -
Bilaterally reacting to light
Left post cataract surgery
Hypotonia + in all 4 limbs
Reflexes-
Bilateral biceps +
Plantars - Mute
Corneal and conjunctival reflexes +
No meningeal signs
Lungs - Bilateral inspiratory crepts in all Lung fields
And expiration wheeze in all Lung fields
Cvs - S1,S2+
Per Abdomen - soft
Bowel sounds +
A -
Altered senorium secondary to ? Hyponatremia
Sepsis secondary to ? cellulitis ? Pyogenic meningitis
? Typhoid
With complete RBBB
P -
Inj.Dexa 4mg iv/ bd
Inj. Ceftriaxone 2 gm iv. Bd
Inj Pantop 40mg IV OD
RT feeds - 100ml milk and 50ml free water 2nd hourly
Investigations :
Hb - 11
TLC - 52500
Pcv - 29.2
Plt - 3.48
TB - 3.46
Db - 0.63
AST - 1036
Alt - 530
TP - 5.3
Alb - 2.73
A/g - 1.06
ABG :
pH - 7.527
pCo2 - 13.7
PO2 - 106
HCo3 - 17.4
Rft :
Urea - 137
Creat - 2.8
uric acid - 11.5
Ca- 10.2
Phosphate - 11.2
Na - 119
K - 4.3
Cl - 75
01/10/21
Icu bed 1
Altered sensorium secondary to hyponatremia
? Pyogenic meningitis
S: Patient sensorium improved and on ventillator CPAP VC mode
O: Bp 110/80 mm hg
Pr 112 bpm
Spo2 99% on fio2 21%
Grbs 120 mg dl
A: Etiology of altered sensorium - Hyponatremia
? Meningoencephalitis
Plan: Extubation
2/10/21
52 year old woman,
ICU bed 1
Pt is drowsy , intermittent spontaneous eye opening present.
O -
GCS E4VTM1
RR - 35 cpm
PR - 88bpm
BP- 110/60mmhg
Temp - 99 F
Spo2 - 98%on T piece (8lot o2)
CNS -
E4VtM1
Pupils -
Bilaterally reacting to light
Left post cataract surgery
Hypotonia + in all 4 limbs
Reflexes-
Bilateral biceps +
Plantars - Mute
Corneal and conjunctival reflexes +
No meningeal signs
Lungs - Bilateral inspiratory crepts in IAA,ISA.
Cvs - S1,S2+
Per Abdomen - soft
Bowel sounds +
A -
Altered senorium secondary to ? Hyponatremia (?SIADH)
? Pyogenic meningitis
?Pre renal aki
Grade 1 bed sore present.
P - To extubate if pt is conscious and maintaining sats .
Inj.Dexa 4mg iv/ bd
Inj. Ceftriaxone 2 gm iv. Bd
Inj Pantop 40mg IV OD
RT feeds - 100ml milk and 50ml free water 4th hourly.
Lft trends in this patient :
3/10/21
S: Patient in ? persistive vegetative state
O : Bp 110/70 mm hg
Pr 70 bpm
Cvs : s1 s2 heard no murmurs
Rs bae
P/a soft
Assesment: Hyponatremia resolved yet patient gcs not improved
Plan: extubation
4/10/21
S: Patient in ? persistive vegetative state.
GCS - E1VtM3
Pupils - NSRL ( left eye post cataract surgery)
O : Bp 140/90 mm hg
Pr 80 bpm
Cvs : s1 s2 heard no murmurs
Rs bae present .
P/a soft
I/O - 2700/1700ml
Assesment: Altered sensorium secondary to Meningitis/hyponatremia .
Hyponatremia secondary to SIADH .
? PYOGENIC MENIGITIS.
ATN /AKI .
? ISCHEMIC / Drug induced hepatitis - resolved.
Grade 2 bed sore.
Plan: Pt maintaining on T piece .
But still not conscious enough for extubation.
Does she require hemo-dilaysis ??
Repeat 2d echo .
ABG :
RFT (YESTERDAY ) - urea - 290 ; creat - 5 ; Na - 125 ; k- 4.3 ; cl- 86 mg/dl. uric acid - 14 (high)
S calcium - 7
corrected ca - 8.6 mg/dl
Qtc prolonged - 537 msec.
06/10/21
S: Patient in ? persistive vegetative state.
GCS - E4VtM1
Pupils - NSRL ( left eye post cataract surgery).
passed stools.
Bed sore increasing ( grade 2 ) .
Pt on Mechanical ventilator - CPAP Vc mode .
pressure support -12 ; peep -5 cmof h20 .
Fio2- 40 %.
Pt also maintaining on T piece intermittently.
O : Bp 110/70 mm hg
Pr 88 bpm.
Spo2- 94%.
Cvs : s1 s2 heard no murmurs
Rs Bae present .
P/a soft
Assesment: Altered sensorium secondary to Meningitis/hyponatremia .
Hyponatremia secondary to SIADH .
? PYOGENIC MENIGITIS.
ATN /AKI - resolving
Grade 2 bed sore.
Hypocalcaemia ( Ionised calcium - 1.94 mg/dl) - very low. - correction was given .
Yesterday rft - Urea - 263 ; creat - 2.9
Na- 130 ; k- 4 .3 ; cl-89.
Creat decreased from 4.8 to 2.9
P- TO extubate.
But she might require tracheostomy mostly.
Cause for hypocalcaemia ?
07/10/21
S: Patient in ? persistive vegetative state.
GCS - E1VtM1
Pupils - NSRL ( left eye post cataract surgery).
passed stools.
Bed sore increasing ( grade 2 ) .(dressing done)
S- Yesterday night , patient saturation were falling on T piece (75-78%) . So immediately oral and ET suction was done , and pt was connected back to ventilator with fio2- 100% .
Meanwhile pt collapsed and her central pulse was absent. So cpr was started according to AHA guidelines.
After 2 Cycles of cpr ,pt revived . She was connected back to mechanical ventilator - ACMV -VC mode .
RR- 14/MIN ; FIO2-100% ; VT -420 ml; PEEP- 5 cm.
of h20 .
Post CPR vitals :
Bp- 80/60 mmhg ( started on noradrenaline@ 4ml/hr)
Pr- 150 bpm ; SPO2- 100% .
Today morning vitals :
O : Bp 120/70 mm hg - on NA @2 ml/hr
Pr -92 bpm.
Spo2- 100%
Cvs : s1 s2 heard no murmurs
Rs Bae present .
P/a soft .
Assesment: Altered sensorium secondary to Meningitis/hyponatremia .
Hyponatremia secondary to SIADH .
? PYOGENIC MENIGITIS.
ATN /AKI - resolving
Grade 2 bed sore.
Hypocalcaemia ( Ionised calcium - 1.94 mg/dl) - very low. - correction was given .
Post cpr status.
Yesterday rft - Urea - 229 ; creat - 2.3
Na- 136 ; k- 4 ; cl-98.
P- TO extubate.
But she might require tracheostomy mostly.
Post cpr ecg - showing rbbb and t wave inversions in v1-v3. Poor r wave progression
lumber puncture done
CSF cell count 2
08/10/21
S: Patient in ? persistive vegetative state.
GCS - E1VtM1
Pupils - NSRL ( left eye post cataract surgery).
passed stools.
Bed sore increasing ( grade 2 ) .(dressing done)
O : Bp 110/70 mm hg
Pr -82 bpm.
Spo2- 98%
Cvs : s1 s2 heard no murmurs
Rs Bae present .
P/a soft
Assesment: Altered sensorium secondary to Meningitis/hyponatremia .
Hyponatremia secondary to SIADH .
? PYOGENIC MENIGITIS.
ATN /AKI - resolving
Grade 2 bed sore.
Hypocalcaemia ( Ionised calcium - 1.94 mg/dl) - very low. - correction was given .
Post cpr status.
Lp done yesterday . Cell count - 2 .; Rbc - nil
Dc - 100% lymphocytes .
Yesterday rft - Urea - 223 ; creat - 2
Na- 135 ; k- 3.9 ; cl-97
P - plan for tracheostomy.
09/10/21
S: Patient in ? persistive vegetative state.
GCS - E2VtM2
Pupils - NSRL ( left eye post cataract surgery).
passed stools.
Bed sore increasing ( grade 2 ) .(dressing done)
Able to move her right fingers intermittently.
O : Bp 140/70 mm hg
Pr -82 bpm.
Spo2- 98%. On SIMV mode - RR- 14/min ; fio2- 40%
peep-5 cm of h20 ; TV-420 ml.
Cvs : s1 s2 heard no murmurs
Rs Bae present .
P/a soft
Assesment: Altered sensorium secondary to Meningitis/hyponatremia .
Hyponatremia secondary to SIADH .
? PYOGENIC MENIGITIS.
ATN /AKI - resolving
Grade 2 bed sore.
Hypocalcaemia ( Ionised calcium - 1.94 mg/dl) - very low. - correction was given .
Post cpr status.
P - plan for tracheostomy today at 9 am .
10/10/21
Tracheostomy POD -DAY 1
S: Patient is conscious ,
GCS - E4V1M4
Pupils - NSRL ( left eye post cataract surgery).
passed stools.
Bed sore increasing ( grade 2 ) .(dressing done)
Able to move her right upper limb and lower limb. Left side no movements noted.
O : Bp 130/70 mm hg
Pr -87 bpm.
Spo2- 95%. Ventilator connected to tracheostomy tube . - On ACMV-VC mode - RR- 14/min ; fio2- 21%
peep-5 cm of h20 ; TV-380 ml.
Cvs : s1 s2 heard no murmurs
Rs Bae present .
P/a soft
GRBS -129 mg/dl
I/O- 3400/2200 ml
CNS - POWER - R. L
• UL- 3/5. 0/5
• . LL -3/5 0/5
• TONE - Decreased all 4 limbs .
• Assesment: Altered sensorium secondary to Meningitis/hyponatremia .
Hyponatremia secondary to SIADH .( resolved).
? PYOGENIC MENIGITIS.
ATN /AKI - resolved
Grade 2 bed sore.
Post cpr status.
Tracheostomy- Pod day 1
Rft - urea - 129 ; s creat - 1 ; Na- 134 ; k-2.7 ; cl-101
hb-8.3 ; tlc - 30k ; plt-1.51
abg - Ph - 7.41 ; pco2- 25 ;po2-112 ; hco3-19.3
P- 2 nd hrly tracheostomy tube suctioning.
Deflate cuff 2nd hrly for 5 min and re-inflate.
11/10/21
Subjectively : patient nodding her head for commands and able to lift her right upper and lower limb
Objectively : pupils Both eys reacting to light
GCS : E4V1M4
Passed stools
No fever spikes
Grbs : 172 mg/dl
I/o : 2600/1600
Bp 140/80 mm hg
Pr : 90 bpm
Spo2 : 100% on 2 L O2 on T piece
Cvs s1 s2 heard no murmurs
Rs bae+
P/a soft nt
Cns : tone decreased in all limbs
Power : 3/5 on right side
0/5 on left upper and lower limbs
Assesment : Altered sensorium secondary to pyogenic meningitis / Hyponatremia (SIADH) resolved
Aki resolved : MODS resolved
Grade 2 bedsore
Post cpr status
Tracheostomy pod 3
Plan : An Mri to rule out ic bleed for ?hemiparesis
12/10/21
At 2:00 am patient suddenly had gasping with ecg showing bradycardia PR:20 cpm and spo2 60 % on ventillator of fio2 90
And patient had no pulse
Cpr was initiated and atropine 1 mg was given and 5 cycles of cpr was done then patient had suctioning was done and mucus plugs were removed
Patient was revived with spo2 of 100%
Pupils dilated fixed
Bp 90/80 mm hg
Pr 160 bpm
Grbs 101 mg/dl
Cvs s1s2 heard
Rs : Bae+
P/a: soft ,NT
Post cpr Abg :
Ph :7.031
Pco2 64.9
Po2:155
Hco3:13.5
Assesment : Bradycardia secondary to hypoxia( ET obstruction with mucus plug)
8::00am
Subjectively : patient comatose
Objectively : pupils Both eys dilated and fixed.
Corneal reflex and conjunctival reflex absent
Dolls eye negative
GCS : E1v1M1
Passed stools
3 fever spikes
Grbs : 172 mg/dl
I/o : 3500/1500
Bp 80/60mm hg
Pr : 90 bpm
Spo2 : 100% on ACMV mode
Fio2 500
Peep 5 cm h2o
Cvs s1 s2 heard no murmurs
Rs bae+
P/a soft nt
Cns : tone decreased in all limbs
Power : 0/5 on right side
0/5 on left upper and lower limbs
Assesment : Altered sensorium secondary to pyogenic meningitis / Hyponatremia (SIADH) resolved
Aki resolved : MODS resolved
Grade 2 bedsore
Post cpr status
Tracheostomy pod 3
?Hypoxic Ischaemic encephalopathy
Plan : suctioning every 2nd hourly
Abg morning ph:7.27
Pco2:54
Po2:38
Hco3:21
Plan : Inj Noradrenaline infusiom 4ml/hr















































Comments
Post a Comment